Electroarthrography to Predict Cartilage Quality
Article by Jackie Zions interviewing Dr. Adele Changoor and Dr. Judith Koenig
Researchers from the Ontario Veterinary College (OVC) and University of Toronto are developing a novel method to measure the quality of cartilage in horses using electroarthrography (EAG). EAG is a non-invasive technique that uses electrodes attached to the skin around a joint to detect electrical signals produced by the cartilage when it is loaded.
Dr. Adele Changoor, from the University of Toronto and Lunenfeld Tanenbaum Research Institute, and Ontario Veterinary College researcher Dr. Judith Koenig from the department of Clinical Studies, explain how EAG works and why it may become very useful for predicting cartilage quality and diagnosing osteoarthritis and other degenerative joints diseases in horses.
EAG is analogous to electrocardiography (ECG), which measures the electrical activity of the heart. Cartilage produces electrical signals during loading and these signals reflect its biomechanical properties, such as stiffness and permeability.
“By measuring EAG signals, we can get an idea of how healthy the cartilage is,” said Changoor.
Healthy cartilage ensures joints can move without pain and has an important role preventing wear and tear on bone.
Currently, there are no readily available tools to assess cartilage quality in horses with the exception of diagnostic arthroscopy – a minimal invasive surgery – under general anesthesia. X-rays and ultrasound are not sensitive enough to detect cartilage changes, and magnetic resonance imaging (MRI) is expensive, requires anesthesia and is often difficult to access. EAG offers a potential alternative that is fast, easy, and affordable.
“EAG is a promising tool for detecting cartilage damage early allowing intervention with treatments that can slow down or prevent further deterioration of the joint,” says Koenig “EAG could also help us monitor the effectiveness of treatments over time.”
EAG measurements were collected at the same time as the center of pressure (COP), which measures the distribution of force under the horse’s hoof when it stands or walks.
“EAG is really tied directly to cartilage biomechanical properties,” says Changoor. “We also needed to know about the joint biomechanics in order to interpret EAG properly.” A custom, portable, force mat was developed by Dr. Changoor’s graduate students that included an array of force sensors to place under the horse’s hoof when measuring EAG.
“Then we can measure how much compressive force or ground reaction force is being exerted on that joint” said Changoor. “COP, is where the ground reaction force is acting. The ground reaction force gives us the total load on the joint. COP lets us figure out where on the hoof or where on the joint surface force is being concentrated.”
COP provides information about the joint biomechanics and the horse’s balance and stability. EAG and COP testing were combined to get a comprehensive picture of the joint health and function in horses with osteoarthritis. Results were compared with MRI imaging and it was found that EAG and COP testing correlated well with MRI and could detect differences in cartilage quality between healthy and osteoarthritic joints.
In the 2023 study involving horses with osteoarthritis in the fetlock joint; the horses were treated with MSCs to decrease inflammation and stimulate tissue healing. The researchers measured EAG, COP, and MRI before and after the treatment to evaluate its impact on cartilage quality.
“We observed that MSCs improved cartilage quality in some horses and EAG and COP testing were able to capture these changes and show the responses to treatment. This suggests that EAG and COP testing could be useful for selecting treatment options for the horse,” says Dr. Koenig. “One of the biggest advantages of EAG is that it seems to correspond with our arthroscopic findings. It can perhaps evaluate the quality of the cartilage or cartilage defects, which we are at the moment only able to evaluate with arthroscopy.”
The researchers plan to conduct further studies in order to validate and refine EAG and COP testing for predicting cartilage quality in equines. They hope that these techniques will become widely available and accessible for veterinarians and horse owners in the future.
“This is an exciting and innovative research project that has the potential to improve the diagnosis and early management of osteoarthritis in horses,” says Dr. Koenig “Osteoarthritis is a major health and welfare issue for horses and their owners, and we need better tools to detect it early and treat it. EAG and COP testing could provide a simple, affordable, and accurate way to assess cartilage quality and joint function in horses.”
Many thanks go to the graduate students who worked tirelessly on the EAG study: Peter Suderman, PhD Candidate in the Department of Materials Science & Engineering at U of T, Jaylon Pascual, undergraduate co-op student finishing her fourth year in the Biomedical Engineering program at U of G, Dr Rodrigo Munevar Luque, Equine Sports Medicine Resident at OVC and PhD Candidate Biomedical Sciences at U of G, Undergraduate Research Assistants in Clinical Studies Ashley Nixon, DVM 25 (OVC) , Pjotr Roest DVM 26 (OVC), and in Biomedical Sciences Axel Koenig Parris HBA 25 (Ivey School of Business, Western University) and Rebecca Mullin BSc OVC 25.
The study was funded by the Equine Guelph Research Fund and the Natural Sciences and Engineering Research Council of Canada (NSERC).
A New Look at Lameness
Words - Jackie Zions (interviewing Dr. Koenig)
Prevention is the ideal when it comes to lameness, but practically everyone who has owned horses has dealt with a lay-up due to an unforeseen injury at some point. The following article will provide tools to sharpen your eye for detecting lameness, review prevention tips and discuss the importance of early intervention. It will also begin with a glimpse into current research endeavouring to heal tendon injuries faster, which has obvious horse welfare benefits and supports horse owners eager to return to their training programs. Dr. Judith Koenig of Ontario Veterinary College (OVC) spends half of her time as a surgeon and teacher with a strong interest in equine sports medicine and rehabilitation, and the other half as a researcher at the OVC.
Lameness is a huge focus for Koenig, whose main interest is in tissue healing. “I think over the past 20 or 30 years we have become very, very good in diagnosing the cause of lameness,” says Koenig. “In the past, we had only radiographs and ultrasound as a diagnostic tool, but by now most referral centers also have MRI available; and that allows us to diagnose joint disease or tendon disease even more. We are much better now [at] finding causes that previously may have been missed with ultrasound.”
Improvements in diagnostics have resulted in increased ability to target treatment plans. With all the different biologics on the market today, Koenig sees a shift in the management of joint disease with more people getting away from steroids as a treatment.
The following list is excerpted from Equine Guelph’s short course on lameness offered on TheHorsePortal.ca. It outlines the different diagnostics available:
Stem Cell Therapy
When asked for the latest news on research she has been involved in, Koenig proclaims, “I'm most excited about the fact that horses are responding well to stem cell treatment—better than I have seen any response to any other drug we have tried so far!”
Koenig has investigated the use of many different modalities to see if they accelerate tissue healing and has studied which cellular pathways are affected. Two recent collaborative studies have produced very exciting findings, revealing future promise for treating equine osteoarthritis with stem cell therapy.
In a safety study, Koenig and her team at the Ontario Veterinary College have shown equine pooled cryopreserved umbilical cord blood, (eCB) MSC, to be safe and effective in treatment of osteoarthritis.
“These cells are the ones harvested from umbilical cord blood at the time of foaling and then that blood is taken to the lab and the stem cells are isolated out of it,” explains Koenig. The stem cells are then put through a variety of tests to make sure they are free of infectious diseases. Once given a clean bill of health, they are expanded and frozen.
The stem cells harvested from multiple donors of equine umbilical cord blood [eCB, (kindly provided by eQcell), MSC] were compared to saline injections in research horses. “This type of cells is much more practical if you have a cell bank,” says Koenig. “You can treat more horses with it, and it’s off the shelf.” There were no systemic reactions in the safety study. Research has also shown no different reactions from sourcing from one donor or multiple donors.
In the second study, 10 million stem cells per vial were frozen for use in healing OA from fetlock chips in horses that were previously conditioned to be fit. After the fetlock chip was created, exercise commenced for six more weeks, and then osteoarthritis was evaluated by MRI for a baseline. Half the horses were treated with the pooled MSC stem cells, and the control group received saline before another month of exercise. Then MRI and lameness exams were repeated, and arthroscopy was repeated to score the cartilage and remove the chip.
Lameness was decreased and cartilage scores were improved in the group that received stem cell therapy at the time of the second look with arthroscopy.
Many diagnostics were utilized during this study. MRIs, X-rays, ultrasounds and weekly lameness evaluations all revealed signs of osteoarthritis in fetlock joints improved in the group treated with (eCB) MSCs. After six weeks of treatment, the arthroscopic score was significantly lower (better cartilage) in the MSC group compared to the control group.
“Using the MRI, we can also see a difference that the horses treated with stem cells had less progression of osteoarthritis, which I think is awesome,” says Koenig. “They were less lame when exercised after the stem cell therapy than the horses that received saline.”
This research group also just completed a clinical trial in client-owned horses diagnosed with fetlock injuries with mild to moderate osteoarthritis changes. The horses were given either 10 million or 20 million stem cells and rechecked three weeks and six weeks after the treatment. Upon re-evaluation, the grade of lameness improved in all the horses by at least one. Only two horses presented a mild transient reaction, which dissipated after 48 hours without any need for antibiotics. The horse’s joints looked normal, with any filling in the joint reduced.
There was no difference in the 18 horses, with nine given 10 million stem cells and the other nine 20 million stem cells; so in the next clinical trial, 10 million stem cells will be used.
The research team is very happy with the results of this first-of-its-kind trial, proving that umbilical cord blood stem cells stopped the progression of osteoarthritis and that the cartilage looked better in the horses that received treatment. The future of stem cell therapy is quite promising!
Rehabilitation
Research has shown adhering to a veterinary-prescribed rehabilitation protocol results in a far better outcome than paddock turn out alone. It is beneficial for tendon healing to have a certain amount of controlled stimulation. “These horses have a much better outcome than the horses that are treated with just being turned out in a paddock for half a year,” emphasizes Koenig. “They do much better if they follow an exercise program. Of course, it is important not to overdo it.”
For example, Koenig cautions against skipping hand-walking if it has been advised. It can be so integral to stimulating healing, as proven in recent clinical trials. “The people that followed the rehab instructions together with the stem cell treatment in our last study—those horses all returned to racing,” said Koenig.
“It is super important to follow the rehab instructions when it comes to how long to rest and not to start back too early.”
Another concern when rehabilitating an injured horse would be administering any home remedies that you haven't discussed with your veterinarian. Examples included blistering an area that is actively healing or applying shockwave to mask pain and then commence exercise.
Prevention and Training Tips
While stating there are many methods and opinions when it comes to training horses, Koenig offered a few common subjects backed by research. The first being the importance of daily turnout for young developing horses.
Turnout and exercise
Many studies have looked at the quality of cartilage in young horses with ample access to turn out versus those without. It has been determined that young horses that lack exercise and are kept in a stall have very poor quality cartilage.
Horses that are started early with light exercise (like trotting short distances and a bit of hill work) and that have access to daily paddock turnout, had much better quality of cartilage. Koenig cited research from Dr. Pieter Brama and similar research groups.
Another study shows that muscle and tendon development depend greatly on low grade exercise in young horses. Evaluations at 18 months of age found that the group that had paddock turnout and a little bit of exercise such as running up and down hills had better quality cartilage, tendon and muscle.
Koenig provides a human comparison, with the example of people that recover quicker from injury when they have been active as teenagers and undergone some beneficial conditioning. The inference can be made that horses developing cardiovascular fitness at a young age stand to benefit their whole lives from the early muscle development.
Koenig says it takes six weeks to regain muscle strength after injury, but anywhere from four to six months for bone to develop strength. It needs to be repeatedly loaded, but one should not do anything too crazy! Gradual introduction of exercise is the rule of thumb.
Rest and Recovery
“Ideally they have two rest days a week, but one rest day a week as a minimum,” says Koenig. “I cannot stress enough the importance of periods of rest after strenuous work, and if you notice any type of filling in the joints after workout, you should definitely rest the horse for a couple of days and apply ice to any structures that are filled or tendons or muscles that are hard.”
Not purporting to be a trainer, Koenig does state that two speed workouts a week would be a maximum to allow for proper recovery. You will also want to make sure they have enough access to salt/electrolytes and water after training.
During a post-Covid interview, Koenig imparted important advice for bringing horses back into work methodically when they have experienced significant time off.
“You need to allow at least a six-week training period for the athletes to be slowly brought back and build up muscle mass and cardiovascular fitness,” says Koenig. “Both stamina and muscle mass need to be retrained.”
Watch video: “Lameness research - What precautions do you take to start training after time off?”
The importance was stressed to check the horse’s legs for heat and swelling before and after every ride and to always pick out the feet. A good period of walking is required in the warmup and cool down; and riders need to pay attention to soundness in the walk before commencing their work out.
Footing and Cross Training
With a European background, Koenig is no stranger to the varying track surfaces used in their training programs. Statistics suggest fewer injuries with horses that are running on turf, like they practice in the UK.
Working on hard track surfaces has been known to increase the chance of injury, but delving into footing is beyond the scope of this article.
“Cross training is very important,” says Koenig. “It is critical for the mental and proper musculoskeletal development of the athlete to have for every three training days a day off, or even better provide cross-training like trail riding on these days."
Cross-training can mitigate overtraining, giving the body and mind a mental break from intense training. It can increase motivation and also musculoskeletal strength. Varied loading from training on different terrain at different gaits means bone and muscle will be loaded differently, therefore reducing repetitive strain that can cause lameness.
Hoof care
Whether it is a horse coming back from injury, or a young horse beginning training, a proficient farrier is indispensable to ensure proper balance when trimming the feet. In fact, balancing the hoof right from the start is paramount because if they have some conformational abnormalities, like abnormal angles, they tend to load one side of their joint or bone more than the other. This predisposes them to potentially losing bone elasticity on the side they load more because the bone will lay down more calcium on that side, trying to make it stronger; but it actually makes the bone plate under the cartilage brittle.
Koenig could not overstate the importance of excellent hoof care when it comes to joint health and advises strongly to invest in a good blacksmith. Many conformational issues can be averted by having a skilled farrier right from the time they are foals. Of course, it would be remiss not to mention that prevention truly begins with nutrition. “It starts with how the broodmare is fed to prevent development of orthopedic disease,” says Koenig. Consulting with an equine nutritionist certainly plays a role in healthy bone development and keeping horses sound.
EIPH - could there be links to sudden death and pulmonary haemorrhage?
Dr Peter W. Physick-Sheard, BVSc, FRCVS, explores preliminary research and hypotheses, being conducted by the University of Guelph, to see if there is a possibility that these conditions are linked and what this could mean for future management and training of thoroughbreds.
"World's Your Oyster,” a three-year-old thoroughbred mare, presented at the veterinary hospital for clinical examination. She won her maiden start as a two-year-old and placed once in two subsequent starts. After training well as a three-year-old, she failed to finish her first start, easing at the top of the stretch, and was observed to fade abruptly during training. Some irregularity was suspected in heart rhythm after exercise. Thorough clinical examination, blood work, ultrasound of the heart and an ECG during rest and workout revealed nothing unusual.
Returning to training, Oyster placed in six of her subsequent eight starts, winning the last two. She subsequently died suddenly during early training as a four-year-old. At post-mortem, diagnoses of pulmonary haemorrhage and exercise-induced pulmonary haemorrhage were established—a very frustrating and unfortunate outcome.
Across the racing world, a case like this probably occurs daily. Anything that can limit a horse's ability to express its genetic potential is a major source of anxiety when training. The possibility of injury and lameness is the greatest concern, but a close second is respiratory disease, with bleeding from the lungs (most often referred to as exercise induced pulmonary [lung] haemorrhage or EIPH) being high on the list.
EIPH is thought to occur in as many as 85 percent of racehorses, and may initially be very mild without obvious clinical consequences. In some cases it can be associated with haemorrhage of sufficient severity for blood to appear at the nostrils, even at first occurrence. In many racing jurisdictions this is a potentially career-ending problem. In these horses, an impact on performance is unquestionable. Bleeding from the lungs is the reason for the existence of ‘Lasix programs,’ involving pre-race administration of a medication considered to reduce haemorrhage. Such programs are controversial—the justifications for their existence ranging from addressing welfare concerns for the horse to dealing with the performance impacts.
Much less frequently encountered is heavy exercise-associated bleeding from the nostrils (referred to as epistaxis), which can sometimes be accompanied by sudden death, during or shortly after exercise. Some horses bleed heavily internally and die without blood appearing at the nostrils. Haemorrhage may only become obvious when the horse is lying on its side, or not until post-mortem. Affected animals do not necessarily have any history of EIPH, either clinically or sub-clinically. There is an additional group of rare cases in which a horse simply dies suddenly, most often very soon after work and even after a winning performance, and in which little to nothing clearly explains the cause on post-mortem. This is despite the fact most racing jurisdictions study sudden death cases very closely.
EIPH is diagnosed most often by bronchoscopy—passing an endoscope into the lung after work and taking a look. In suspected but mild cases, there may not be sufficient haemorrhage to be visible, and a procedure called a bronchoalveolar lavage is performed. The airways are rinsed and fluid is collected and examined microscopically to identify signs of bleeding. Scoping to confirm diagnosis is usually a minimum requirement before a horse can be placed on a Lasix program.
Are EIPH, severe pulmonary haemorrhage and sudden death related? Are they the same or different conditions?
At the University of Guelph, we are working on the hypothesis that most often they are not different—that it’s degrees of the same condition, or closely related conditions perhaps with a common underlying cause. We see varying clinical signs as being essentially a reflection of severity and speed of onset of underlying problems.
Causes in individual cases may reflect multiple factors, so coming at the issues from several different directions, as is the case with the range of ongoing studies, is a good way to go so long as study subjects and cases are comparable and thoroughly documented. However, starting from the hypothesis that these may all represent basically the same clinical condition, we are approaching the problem from a clinical perspective, which is that cardiac dysfunction is the common cause.
Numerous cardiac disorders and cellular mechanisms have the potential to contribute to transient or complete pump (heart) failure. However, identifying them as potential disease candidates does not specifically identify the role they may have played, if any, in a case of heart failure and in lung haemorrhage; it only means that they are potential primary underlying triggers. It isn't possible for us to be right there when a haemorrhage event occurs, so almost invariably we are left looking at the outcome—the event of interest has passed. These concerns influence the approach we are taking.
Background
The superlative performance ability of a horse depends on many physical factors:
Huge ventilatory (ability to move air) and gas exchange capacity
Body structure including limb length and design - allows it to cover ground rapidly with a long stride
Metabolic adaptations - supports a high rate of energy production by burning oxygen, tolerance of severe metabolic disruptions toward the end of race-intensity effort
High cardiovascular capacity - allows the average horse to pump roughly a brimming bathtub of blood every minute
At race intensity effort, these mechanisms, and more, have to work in coordination to support performance. There is likely not much reserve left—two furlongs (400m) from the winning post—even in the best of horses. There are many wild cards, from how the horse is feeling on race day to how the race plays out; and in all horses there will be a ceiling to performance. That ceiling—the factor limiting performance—may differ from horse to horse and even from day to day. There’s no guarantee that in any particular competition circumstances will allow the horse to perform within its own limitations. One of these factors involves the left side of the heart, from which blood is driven around the body to the muscles.
A weak link - filling the left ventricle
The cardiovascular system of the horse exhibits features that help sustain a high cardiac output at peak effort. The feature of concern here is the high exercise pressure in the circulation from the right ventricle, through the lungs to the left ventricle. At intense effort and high heart rates, there is very little time available to fill the left ventricle—sometimes as little as 1/10 of a second; and if the chamber cannot fill properly, it cannot empty properly and cardiac output will fall. The circumstances required to achieve adequate filling include the readiness of the chamber to relax to accept blood—its ‘stiffness.’ Chamber stiffness increases greatly at exercise, and this stiffened chamber must relax rapidly in order to fill. That relaxation seems not to be sufficient on its own in the horse at high heart rates. Increased filling pressure from the circulation draining the lungs is also required. But there is a weak point: the pulmonary capillaries.
These are tiny vessels conducting blood across the lungs from the pulmonary artery to the pulmonary veins. During this transit, all the gas exchange needed to support exercise takes place. The physiology of other species tells us that the trained lung circulation achieves maximum flow (equivalent to cardiac output) by reducing resistance in those small vessels. This process effectively increases lung blood flow reserve by, among other things, dilating small vessels. Effectively, resistance to the flow of blood through the lungs is minimised. We know this occurs in horses as it does in other species; yet in the horse, blood pressure in the lungs still increases dramatically at exercise.
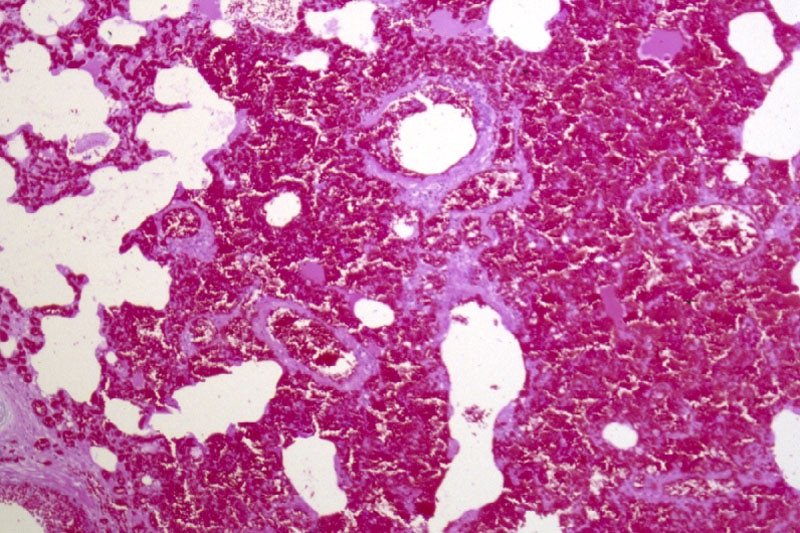
If this increase is not the result of resistance in the small vessels, it must reflect something else, and that appears to be resistance to flow into the left chamber. This means the entire lung circulation is exposed to the same pressures, including the thin-walled capillaries. Capillaries normally work at quite low pressure, but in the exercising horse, they must tolerate very high pressures. They have thin walls and little between them, and the air exchange sacs in the lung. This makes them vulnerable. It's not surprising they sometimes rupture, resulting in lung haemorrhage.
Recent studies identified changes in the structure of small veins through which the blood flows from the capillaries and on toward the left chamber. This was suspected to be a pathology and part of the long-term consequences of EIPH, or perhaps even part of the cause as the changes were first identified in EIPH cases. It could be, however, that remodelling is a normal response to the very high blood flow through the lungs—a way of increasing lung flow reserve, which is an important determinant of maximum rate of aerobic working.
The more lung flow reserve, the more cardiac output and the more aerobic work an animal can perform. The same vein changes have been observed in non-racing horses and horses without any history or signs of bleeding. They may even be an indication that everything is proceeding as required and a predictable consequence of intense aerobic training. On the other hand, they may be an indication in some horses that the rate of exercise blood flow through their lungs is a little more than they can tolerate, necessitating some restructuring. We have lots to learn on this point.
If the capacity to accommodate blood flow through the lungs is critical, and limiting, then anything that further compromises this process is likely to be of major importance. It starts to sound very much as though the horse has a design problem, but we shouldn't rush to judgement. Horses were probably not designed for the very intense and sustained effort we ask of them in a race. Real-world situations that would have driven their evolution would have required a sprint performance (to avoid ambush predators such as lions) or a prolonged slower-paced performance to evade predators such as wolves, with only the unlucky victim being pushed to the limit and not the entire herd.
Lung blood flow and pulmonary oedema
There is another important element to this story. High pressures in the capillaries in the lung will be associated with significant movement of fluid from the capillaries into lung tissue spaces. This movement in fact happens continuously at all levels of effort and throughout the body—it's a normal process. It's the reason the skin on your ankles ‘sticks’ to the underlying structures when you are standing for a long time. So long as you keep moving a little, the lymphatic system will draw away the fluid.
In a diseased lung, tissue fluid accumulation is referred to as pulmonary oedema, and its presence or absence has often been used to help characterise lung pathologies. The lung lymphatic system can be overwhelmed when tissue fluid is produced very rapidly. When a horse experiences sudden heart failure, such as when the supporting structures of a critical valve fail, one result is massive overproduction of lung tissue fluid and appearance of copious amounts of bloody fluid from the nostrils.
The increase in capillary pressure under these conditions is as great as at exercise, but the horse is at rest. So why is there no bloody fluid in the average, normal horse after a race? It’s because this system operates very efficiently at the high respiratory rates found during work: tissue fluid is pumped back into the circulation, and fluid does not accumulate. The fluid is pumped out as quickly as it is formed. An animal’s level of physical activity at the time problems develop can therefore make a profound difference to the clinical signs seen and to the pathology.
Usual events with unusual consequences
If filling the left ventricle and the ability of the lungs to accommodate high flow at exercise are limiting factors, surely this affects all horses. So why do we see such a wide range of clinical pictures, from normal to subclinical haemorrhage to sudden death?
Variation in contributing factors such as type of horse, type and intensity of work, sudden and unanticipated changes in work intensity, level of training in relation to work and the presence of disease states are all variables that could influence when and how clinical signs are seen, but there are other considerations.
Although we talk about heart rate as a fairly stable event, there is in fact quite a lot of variation from beat to beat. This is often referred to as heart rate variability. There has been a lot of work performed on the magnitude of this variability at rest and in response to various short-term disturbances and at light exercise in the horse, but not a lot at maximal exercise. Sustained heart rate can be very high in a strenuously working horse, with beats seeming to follow each other in a very consistent manner, but there is in fact still variation.
Some of this variation is normal and reflects the influence of factors such as respiration. However, other variations in rate can reflect changes in heart rhythm. Still other variations may not seem to change rhythm at all but may instead reflect the way electrical signals are being conducted through the heart.
These may be evident from the ECG but would not appear abnormal on a heart rate monitor or when listening. These variations, whether physiologic (normal) or a reflection of abnormal function, will have a presently, poorly understood influence on blood flow through the lungs and heart—and on cardiac filling. Influences may be minimal at low rates, but what happens at a heart rate over 200 and in an animal working at the limits of its capacity?
Normal electrical activation of the heart follows a pattern that results in an orderly sequence of heart muscle contraction, and that provides optimal emptying of the ventricles. Chamber relaxation complements this process.
An abnormal beat or abnormal interval can compromise filling and/or emptying of the left ventricle, leaving more blood to be discharged in the next cycle and back up through the lungs, raising pulmonary venous pressure. A sequence of abnormal beats can lead to a progressive backup of blood, and there may not be the capacity to hold it—even for one quarter of a second, a whole cardiac cycle at 240 beats per minute.
For a horse that has a history of bleeding and happens to be already functioning at a very marginal level, even minor disturbances in heart rhythm might therefore have an impact. Horses with airway disease or upper airway obstructions, such as roarers, might find themselves in a similar position. An animal that has not bled previously might bleed a little, one that has a history of bleeding may start again, or a chronic bleeder may worsen.
Relatively minor disturbances in cardiac function, therefore, might contribute to or even cause EIPH. If a horse is in relatively tough company or runs a hard race, this may also contribute to the onset or worsening of problems. Simply put, it's never a level playing field if you are running on the edge.
Severe bleeding
It has been suspected for many years that cases of horses dying suddenly at exercise represent sudden-onset cardiac dysfunction—most likely a rhythm disturbance. If the rhythm is disturbed, the closely linked and carefully orchestrated sequence of events that leads to filling of the left ventricle is also disturbed. A disturbance in cardiac electrical conduction would have a similar effect, such as one causing the two sides of the heart to fall out of step, even though the rhythm of the heart may seem normal.
The cases of horses that bleed profusely at exercise and even those that die suddenly without any post-mortem findings can be seen to follow naturally from this chain of events. If the changes in heart rhythm or conduction are sufficient, in some cases to cause massive pulmonary haemorrhage, they may be sufficient in other cases to cause collapse and death even before the horse has time to exhibit epistaxis or even clear evidence of bleeding into the lungs.
EIPH and dying suddenly
If these events are (sometimes) related, why is it that some horses that die of pulmonary haemorrhage with epistaxis do not show evidence of chronic EIPH? This is one of those $40,000 questions. It could be that young horses have had limited opportunity to develop chronic EIPH; it may be that we are wrong and the conditions are entirely unrelated. But it seems more likely that in these cases, the rhythm or conduction disturbance was sufficiently severe and/or rapid in onset to cause a precipitous fall in blood pressure with the animal passing out and dying rapidly.
In this interpretation of events, the missing link is the heart. There is no finite cutoff at which a case ceases to be EIPH and becomes pulmonary haemorrhage. Similarly, there is no distinct point at which any case ceases to be severe EIPH and becomes EAFPH (exercise-associated fatal pulmonary haemorrhage). In truth, there may simply be gradation obscured somewhat by variable definitions and examination protocols and interpretations.
The timing of death
It seems from the above that death should most likely take place during work, and it often does, but not always. It may occur at rest, after exercise. Death ought to occur more often in racing, but it doesn't.
The intensity of effort is only one factor in this hypothesis of acute cardiac or pump failure. We also have to consider factors such as when rhythm disturbances are most likely to occur (during recovery is a favourite time) and death during training is more often a problem than during a race.
A somewhat hidden ingredient in this equation is possibly the animal's level of emotional arousal, which is known to be a risk factor in humans for similar disturbances. There is evidence that emotions/psychological factors might be much more important in horses than previously considered. Going out for a workout might be more stimulating for a racehorse than a race because before a race, there is much more buildup and the horse has more time to adequately warm up psychologically. And then, of course, temperament also needs to be considered. These are yet further reasons that we have a great deal to learn.
Our strategy at the University of Guelph
These problems are something we cannot afford to tolerate, for numerous reasons—from perspectives of welfare and public perception to rider safety and economics. Our aim is to increase our understanding of cardiac contributions by identifying sensitive markers that will enable us to say with confidence whether cardiac dysfunction—basically transient or complete heart failure—has played a role in acute events.
We are also looking for evidence of compromised cardiac function in all horses, from those that appear normal and perform well, through those that experience haemorrhage, to those that die suddenly without apparent cause. Our hope is that we can not only identify horses at risk, but also focus further work on the role of the heart as well as the significance of specific mechanisms. And we hope to better understand possible cardiac contributions to EIPH in the process. This will involve digging deeply into some aspects of cellular function in the heart muscle, the myocardium of the horse, as well as studying ECG features that may provide insight and direction.
Fundraising is underway to generate seed money for matching fund proposals, and grant applications are in preparation for specific, targeted investigations. Our studies complement those being carried out in numerous, different centres around the world and hopefully will fill in further pieces of the puzzle. This is, indeed, a huge jigsaw, but we are proceeding on the basis that you can eat an elephant if you're prepared to process one bite at a time.
How can you help? Funding is an eternal issue. For all the money that is invested in horses there is a surprisingly limited contribution made to research and development—something that is a mainstay of virtually every other industry; and this is an industry.
Look carefully at the opportunities for you to make a contribution to research in your area. Consider supporting studies by making your experience, expertise and horses available for data collection and minimally invasive procedures such as blood sampling.
Connect with the researchers in your area and find out how you can help. Watch your horses closely and contemplate what they might be telling you—it's easy to start believing in ourselves and to stop asking questions. Keep meticulous records of events involving horses in your care— you never know when you may come across something highly significant. And work with researchers (which often includes track practitioners) to make your data available for study.
Remember that veterinarians and university faculty are bound by rules of confidentiality, which means what you tell them should never be ascribed to you or your horses and will only be used without any attribution, anonymously. And when researchers reach out to you to tell you what they have found and to get your reactions, consider actually attending the sessions and participating in the discussion; we can all benefit—especially the ultimate beneficiary which should be the horse. We all have lots to learn from each other, and finding answers to our many challenges is going to have to be a joint venture.
Finally, this article has been written for anybody involved in racing to understand, but covering material such as this for a broad audience is challenging. So, if there are still pieces that you find obscure, reach out for help in interpretation. The answers may be closer than you think!
Oyster
And what about Oyster? Her career was short. Perhaps, had we known precisely what was going on, we might have been able to treat her, or at least withdraw her from racing and avoid a death during work with all the associated dangers—especially to the rider and the associated welfare concerns.
Had we had the tools, we might have been able to confirm that whatever the underlying cause, she had cardiac problems and was perhaps predisposed to an early death during work. With all the other studies going on, and knowing the issue was cardiac, we might have been able to target her assessment to identify specific issues known to predispose.
In the future, greater insight and understanding might allow us to breed away from these issues and to better understand how we might accommodate individual variation among horses in our approaches to selection, preparation and competition. There might be a lot of Oysters out there!
For further information about the work being undertaken by the University of Guelph
Contact - Peter W. Physick-Sheard, BVSc, FRCVS.
Professor Emeritus, Ontario Veterinary College, University of Guelph - pphysick@uoguelph.ca
Research collaborators - Dr Glen Pyle, Professor, Department of Biomedical Sciences, University of Guelph - gpyle@uoguelph.ca
Dr Amanda Avison, PhD Candidate, Department of Biomedical Sciences, University of Guelph. ajowett@uoguelph.ca
References
Caswell, J.I. and Williams K.J. (2015), Respiratory System, In ed. Maxie, M. Grant, 3 vols., 6th edn., Jubb, Kennedy and Palmer’s Pathology of Domestic Animals, 2; London: Elsevier Health Sciences, 490-91.
Hinchcliff, KW, et al. (2015), Exercise induced pulmonary hemorrhage in horses: American College of Veterinary Internal Medicine consensus statement, J Vet Intern Med, 29 (3), 743-58.
Rocchigiani, G, et al. (2022), Pulmonary bleeding in racehorses: A gross, histologic, and ultrastructural comparison of exercise-induced pulmonary hemorrhage and exercise-associated fatal pulmonary hemorrhage, Vet Pathol, 16:3009858221117859. doi: 10.1177/03009858221117859. Online ahead of print.
Manohar, M. and T. E. Goetz (1999), Pulmonary vascular resistance of horses decreases with moderate exercise and remains unchanged as workload is increased to maximal exercise, Equine Vet. J., (Suppl.30), 117-21.
Vitalie, Faoro (2019), Pulmonary Vascular Reserve and Aerobic Exercise Capacity, in Interventional Pulmonology and Pulmonary Hypertension, Kevin, Forton (ed.), (Rijeka: IntechOpen), Ch. 5, 59-69.
Manohar, M. and T. E. Goetz (1999), Pulmonary vascular resistance of horses decreases with moderate exercise and remains unchanged as workload is increased to maximal exercise, Equine Vet. J., (Suppl.30), 117-21.
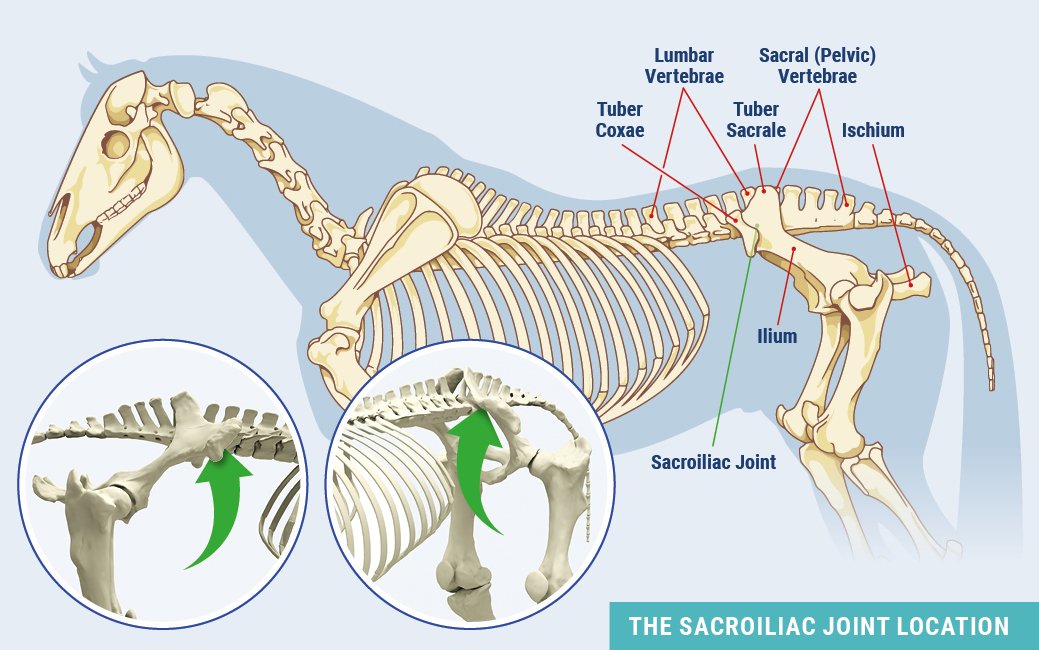
The Often Overlooked Equine Sacroiliac Joint
Horses that present as sore in the hindquarters can be perplexing to diagnose. Sometimes the problem is found in the last place you look – the sacroiliac joint.
Article by Annie Lambert
Even though the sacroiliac joint (SI) was on veterinary radars long ago, due to its location buried under layers of muscle in the equine pelvic region, the joint and surrounding ligaments were tough to diagnose and treat.
The sacroiliac joint is often a source of lower back discomfort in race and performance horses. Trainers may notice several clinical signs of a problem. These hints include sensitivity to grooming, objections to riders getting legged up, stiffness of motion, pain to manual palpation of the rump or back, resistance to being shod behind and poor performance.
Of course, those symptoms could describe other hind limb soundness issues, making the origin of the problem arduous to ascertain. A thorough physical examination with complete therapeutic options can relieve sacroiliac pain. The treatments are complicated, however, by the anatomy of the SI area.
The equine pelvis is composed of three fused bones: ilium, ischium and pubis. The sacrum, the lower part of the equine back, is composed of five fused vertebrae. The sacroiliac joint is located where the sacrum passes under the top of the pelvis (tubera sacrale). The dorsal, ventral and interosseous sacroiliac ligaments help strengthen the SI joint.
The SI and surrounding ligaments provide support during weight bearing, helping to transfer propulsive forces of the hind limbs to the vertebral column—creating motion much like the thrust needed to break from the starting gate.
Sound complicated? It certainly can be.
Diagnosing Dilemmas
It wasn’t until modern medical technology advanced that the SI could be explored seriously as a cause of hind lameness.
“The sacroiliac is one of the areas that’s very hard to diagnose or image,” explained Dr. Michael Manno, a senior partner of San Dieguito Equine Group in San Marcos, California. “[Diagnostics] of the area probably correlated with bone scans or nuclear scintigraphy. You can’t really use radiographs because the horse is so massive and there is so much muscle, you can’t get a good image.
“About the only time you can focus on the pelvis and get a decent radiograph is if the horse is anesthetized—you have a big [x-ray] machine and could lay the horse down. But, it’s hard because with anything close to a pelvic injury, the last thing you want to do is lay them down and have them have to get back up.”
The nuclear scintigraphs give a good image of hip, pelvis and other anatomical structures buried deep in the equine body, according to Manno, a racetrack practitioner. “Those images can show areas of inflammation that could pretty much be linked right to the SI joint.”
The other modern technological workhorse in the veterinary toolbox is the digital ultrasound machine. Manno pointed out that veterinarians improved diagnostics as they improved their ultrasounding skills and used those skills to ultrasound areas of the body they never thought about before. Using different techniques, frequencies and various heads on the machine’s probe, the results can be fairly remarkable.
“The ultrasound showed you could really image deeper areas of the body, including an image of the sacroiliac joint,” Manno said. “It can also show some ligament issues.”
Where the SI is buried under the highest point of a horse’s rump, and under heavy gluteal muscles, there are two sets of ligaments that may sustain damage and cause pain. The dorsal sacroiliac ligaments do not affect the sacroiliac joint directly, but help secure the ilium to the sacral spine. The ventral sacroiliac ligaments lie deeper, in the sacroiliac joint area, which they help stabilize. These hold the pelvis tight against its spine. The joint itself, being well secured by these ligaments, has little independent movement and therefore contains only minimal joint fluid.
Diagnosing the SI can be complex because horses often travel their normal gait with no change from normal motion—no signs of soreness. Other horses, however, are sore on one leg or another to varying degrees, sometimes with a perceptible limp.
“I don’t know that there is a specific motion,” Manno explained. “You just know that you have a hind end lameness, and I think a lot of performance horses have mildly affected SI joints.
“The horses that are really severe become acutely lame behind, very distinct. You go through the basic diagnostics, and I think most of these horses will show you similar signs as other issues behind. We palpate along the muscles on either side of their spine and they are sore, or you palpate over their croup and you can get them to drop down—that kind of thing. Other times you do an upper limb flexion on them and they might travel weird on the opposite leg. So, it can be a little confusing.”
In the years prior to the early 2000s, the anatomical location of the SI hindered a definite diagnosis; decisions on hind soreness were more of a shrug, “time and rest” treatment evaluation. As one old-time practitioner called it, a SWAG – “Scientific Wild Ass Guess.”
Even with modern tools, making a conclusive diagnosis can be opaque.
“The less affected horses, through exercise and with medications like Robaxin [muscle relaxer] or mild anti-inflammatories, seem to be able to continue to perform,” Manno said. “I don’t know how you can be perfectly sure of an inside joint unless you try to treat it and get results.”
“That’s why bone scans came into play and are really helpful,” Manno added. “You can image that [SI] area from different angles with the machine right over the path of the pelvis, looking down on it or an angle view into it, and then you see it from the side and the back very often. We can get an idea from the different views and angles of where the inflammation is and pinpoint the problem from that.”
Once Manno has a generalized idea of where the problem is, he fine-tunes his hypothesis using more diagnostics with a digital ultrasound machine.
“You can ultrasound from up above and see the joint that way,” he said. “As ultrasound has progressed, we’ve found that the rectal probes the breeding vets have used can also be tuned in to start looking for other things. If you turn them upwards, you can look at the bottom of the pelvis and the SI joint. You can see things through the rectum by just looking straight up. That is a whole new thing that we probably never thought about doing. I don’t profess to be very great at it; it’s not something I do a lot, but there are people that are just wonderful at it.”
Treating a Theorem
But, if the diagnosis is incorrect, the prescribed treatment may be anything but helpful.
“In many cases, if a horse is really sore, you need to be very careful,” cautioned Manno. “What you don’t want to do is go from a strain or some sort of soft tissue injury into a pelvic fracture by trying to keep them going. In many cases you are back in the old rest and time type of treatment.”
Manno pointed out one treatment that has advanced over many years is injecting the SI joint directly. There are a couple of techniques used when injecting the SI. With a blind injection the practitioner directs a long, straight needle into the joint by relying solely on equine anatomy. The other technique employs an ultrasound machine to guide the placement of the needle into the joint.
“Normally we are just injecting cortisone in those cases,” Manno noted. “We are trying to get the inflammatory response to settle down. Hopefully that gives the horse some relief so that they’re a bit more relaxed in their musculature. You know how it is when you get a sore back; it’s hard to keep yourself from cramping, which makes everything worse.”
A slight tweak of that technique is to use a curved needle. When you are positioning the curved needle, it follows the curve of the horse’s anatomy and helps the practitioner direct the injection into the joint.
“It curves right into position for you; it gives you a little help,” Manno confirmed of the curved needle. “Some people are really good with that technique; others still like to go to the straight needle. [The curved needle] helps you approach the site without interference from the bones in that area.”
SI joint injuries affect most performance horses, including Standardbred trotters and pacers, Western performance athletes as well as hunters, jumpers and dressage horses.
The older show horses are often diagnosed with chronic SI pain, sometimes complicated by arthritis. These chronic cases—and admittedly some racehorses—are treated with different therapies. These conservative, nonsurgical treatments have been proven effective.
In addition to stall rest and anti-inflammatories, physical training programs can be useful in tightening the equine patient’s core and developing the topline muscles toward warding off SI pain. Manno, a polo player who also treats polo ponies, believes the hard-working ponies avoid having many SI injuries due to their fitness levels.
“I think these polo horses are similar to a cross between a racehorse and a cutting horse,” Manno opined. “They are running distances and slide stopping and turning.”
Other treatments utilized include shockwave, chiropractic, acupuncture, therapeutic laser and pulsed electromagnetic therapy.
Superior Science
With the new diagnostic tools and advanced protocols in their use, veterinarians can pinpoint the SI joint and surrounding areas much closer. This gives them an improved indication that there definitely is an issue with the sacroiliac.
When there is a question about what is causing hind end lameness, most practitioners begin with blocking from the ground up.
“In many cases with hind end lameness that we can’t figure out, we block the lower leg; if it doesn’t block out down low, we conclude the problem is up high,” Manno said. “Once you get up to the hock you’re out of options of what you can figure out. You start shooting some x-rays, but by the time you get to the stifle, you’re limited. Bone scans and ultrasounds have certainly helped us with diagnosing.”
Manno doesn’t see a lot of SI joint injuries in his practice, but he noted there were cases every now and again. He also opined that there were probably other cases that come up in racehorses on a short-term basis. He also noted that, although it may not be a real prominent injury, that’s not to say it has not gone undiagnosed.
“I think we realize, in many of the horses we treat, that the SI joint is something that may have been overlooked in the past,” Manno concluded. “We just didn’t have the ability to get any firm diagnosis in that area.”